Before discussing subclinical hypocalcemia, it is helpful to review the more obvious disease of clinical hypocalcemia, or what everyone knows as milk fever. This disease can occur in mature dairy cows within three days after calving.
Due to the cow’s progressive loss of calcium to the calf for bone formation and sudden loss for milk production (especially if she is a high producer), her serum calcium levels decline 40% to 80% along with decreases in serum magnesium and phosphorus.
Cows with milk fever initially show signs of excitability and restlessness, walk unsteadily, have muscle and ear twitching, and bellow. At this point, the calcium level is probably less than or equal to 5 milligrams per deciliter. If the level drops below 3 milligrams per deciliter, cows are unable to stand, go off feed, cannot urinate or pass manure and feel cold to the touch. Eventually, they are completely unresponsive and can die.
Such cows need intravenous calcium as soon as possible. Usually, veterinarians administer this treatment while carefully monitoring heart rate and rhythm, as calcium is toxic to the heart muscle. Some cows benefit from phosphorus and magnesium solutions as well or need multiple treatments.
Cows with a history of milk fever, or those who are suspected to get it or even showing early signs, should be given oral calcium in a bolus or propylene glycol gel form. It is also a good idea to delay milking right after calving or at least not milk out completely.
Based on the National Animal Health Management Systems data, about 5% of dairy cows have clinical hypocalcemia at some point. However, there are plenty of cows standing around looking alert but maybe just a little off feed after calving. Studies show that about 47% of multiparous cows have calcium levels less than or equal to about 8 milligrams per deciliter, and if they have those levels for three days after calving, they are considered to be chronic subclinical hypocalcemic.
We know why this happens, as within two days after calving, the energy needs of a cow more than doubles due to production of colostrum and milk. The energy needs are so great most dairy cows do not eat enough to make up for lost calories. This creates a negative energy balance. Of course, bunk space, quality of feed, water availability and opportunities to eat are all important parts of nutrition and management. But sometimes negative energy balance still happens, which can lead to inability to regulate calcium, increased production of lipids and even ketosis.
While other parameters change with a negative energy balance, such as an increase in non-esterified fatty acids, increased beta-hydroxybutyrate and increased vitamin D, calcium is a fairly easy parameter to measure.
In a study of 1,462 cows over 48 hours after calving, 25% to 54% of cows had subclinical hypocalcemia based on calcium testing (Table 1).
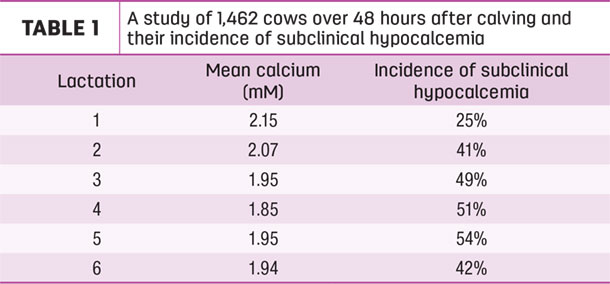
As the number of lactations increased, the greater the percentage of cases. And as the number of lactations increased, the mean calcium decreased. There were fewer cows in this study after the fourth or fifth lactation.
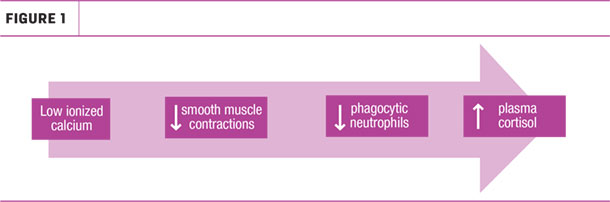
Low ionized calcium impairs normal smooth muscles and decreases phagocytic neutrophils, leading to increased plasma cortisol (Figure 1).
There have been studies on the effects of subclinical hypocalcemia in that not only does reduced calcium lead to altered metabolism, but it also leads to impaired immune function, which of course can make cows susceptible to infections and decreased fertility (Figure 2).
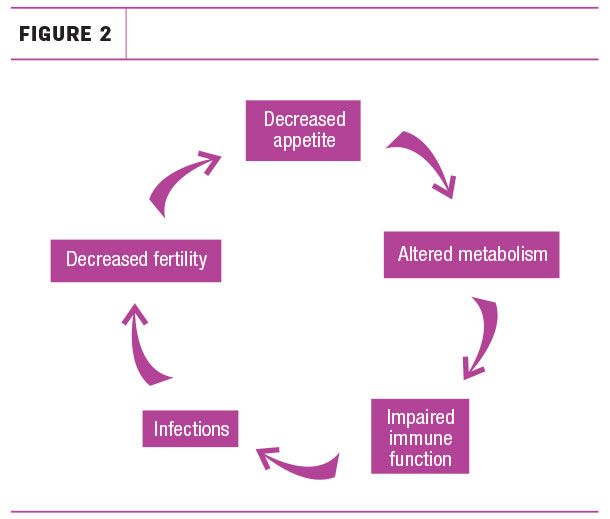
Perhaps increased cortisol is not compatible with fertility. In one study, the percent of cows pregnant at first service after calving was significantly decreased when they had subclinical hypocalcemia. This costs the producer money in repeat A.I. and pregnancy checks.
In another study, the incidence of metritis was significantly greater for cows with subclinical hypocalcemia than for those with normal calcium levels after calving, regardless of their overall risk of metritis due to other factors.
Other studies have looked at incidence of displaced abomasum, ketosis, retained placenta and again at metritis, and found that cows with hypocalcemia are three to 5.5 times more likely to have these conditions, compared to cows with normal calcium. Due to possible increased incidence of metabolic or infection diseases in cows with subclinical hypocalcemia, testing fresh cows’ calcium level will help determine the “herd alarm” for hypocalcemia. The prevalence of these diseases is calculated as the number of cases divided by the number of fresh cows per month. Consider Table 2 from the University of Minnesota Extension related to herd alarm and cost per case.
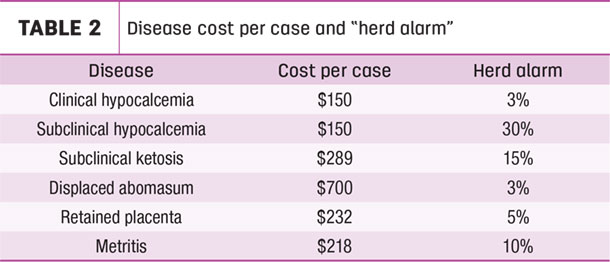
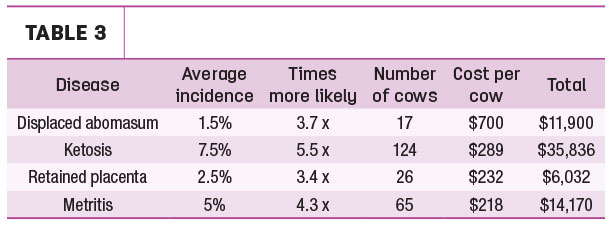
Let’s consider a theoretical herd of 1000 milking cows. If 30% of these cows have subclinical hypocalcemia (not even clinical hypocalcemia), that would be 300 cows. Assume this particular herd has half the “herd alarm” cases of ketosis, displaced abomasum, retained placenta and metritis. Figuring how much more likely it is for the 300 cows with subclinical hypocalcemia to have these other conditions, it is easy to do a rough calculation on the additional expense for these 300 cows not even showing clinical signs of hypocalcemia.
As seen on Table 3, the total extra cost is $67,938 or $226.46 per cow. This does not include repeat A.I. services for cows with subclinical hypocalcemia.
If a basic portable calcium test costs about $5 and calcium boluses cost about $15 for two treatments, that $20 spent is better than a potential of $226.46 per cow. What does this mean for your farm? Look for a herd threshold of subclinical hypocalcemia in order to make the necessary changes to nutrition and management. It is all about prevention, and prevention means knowing where the herd stands.
PHOTO: Photo by Jenna Hurty.
Learn more in this webinar: Arkray





