Editor’s note: This article is the first in a two-part series about how transition cows’ immune systems are impacted by metabolic factors. Read part 2 More metabolic factors affecting the immune system of the transition diary cow. The transition from pregnant, non-lactating to non-pregnant, lactating is too often a disastrous experience for the cow.
Most of the metabolic diseases of dairy cows – milk fever, ketosis, retained placenta and displacement of the abomasum – occur within the first two weeks of lactation.
In addition to metabolic disease, the majority of infectious disease experienced by the dairy cow, especially mastitis and metritis, but also more insidious diseases such as Johne’s disease and salmonellosis, become clinically apparent during the first two weeks of lactation. These diseases are largely due to a poorly functioning immune system.
The first response of the body to an invading pathogen is to send white blood cells known as neutrophils into the area to fight off the infection. If you have had a splinter in a finger, the pus that surrounds the splinter is made up of millions of these neutrophils.
These cells will try to phagocytize (eat) the bacteria and will use various enzymes to kill the bacteria. This is called innate immunity, as the cow is born with this ability. However, if the neutrophils cannot kill the invader, the neutrophils can call for reinforcements. The cells that respond next are macrophages and lymphocytes.
The macrophages may be able to phagocytize the bacteria and kill them, or they may help the lymphocytes respond to the invader. Over the course of seven to 11 days, the lymphocytes will learn to recognize that bacteria and begin producing large amounts of antibody.
This can help to kill the bacteria also. The lymphocytes will also begin to recruit killer lymphocytes that produce various other substances to handle the infection. The “trained” lymphocytes will remember their encounter with the pathogen and will respond to the next infection caused by that bacteria (or virus) much more quickly. This is known as cell-mediated immunity.
The neutrophils and lymphocytes can be isolated from a cow’s blood and tested for their ability to kill invading bacteria or for the ability to produce antibody. Dr. Marcus Kehrli at the USDA, and Dr. James Roth at Iowa State University, demonstrated neutrophil and lymphocyte function decline in cows about two weeks before calving.
Immune cell function will reach a low point at calving; on average there is a 25 to 30 percent decline in function. Full function of the cells is not restored until the average cow is two to three weeks into lactation. Being an average, that means some cows exhibit almost no decline in function around the time of calving, and some cows have a terrible loss of function.
A number of studies have demonstrated that a weak immune system makes the cow more susceptible to mastitis, metritis and even retained placenta. There is evidence the neutrophils have a role in separation of fetal placenta from maternal caruncles of the uterus.
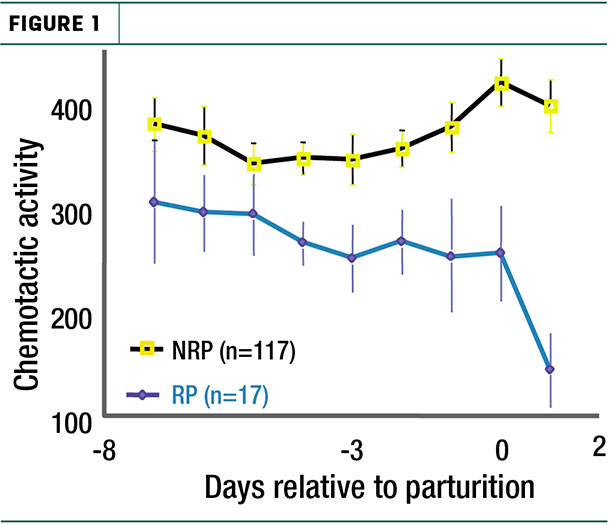
When they fail to separate, the cow develops a retained placenta. Dr. Kayoko Kimura, working at the USDA National Animal Disease Center, showed that the ability of neutrophils to attack placental tissue was greatly reduced three to four days before calving in cows that were going to develop a retained placenta (Figure 1).
Metritis and immune suppression
Upon delivery of a calf, the cervical canal remains open for a period of days. This allows fluids and tissue no longer required to maintain pregnancy to leave the uterus. It also permits bacteria to ascend the vagina and gain entry to the uterus. Bacteria can be isolated from the uterus of most cows during the first week after calving.
In most cows, neutrophils react to the initial bacterial invasion by moving from the blood into the lumen of the uterus to fight the bacteria and eliminate the bacterial infection. The infection remains low-grade or subclinical. The cow remains “healthy” and goes on her way toward a productive lactation and subsequent pregnancy.
However, in from 15 to 30 percent of cows, the neutrophils have lost enough function they do not successfully halt the infection. In these animals, bacterial populations explode, causing metritis. The high bacterial numbers causes an even larger inflammatory response to these bacteria and results in a purulent, fetid discharge referred to as metritis. Upon rectal palpation, the uterus is enlarged and the inflammation of the uterus suppresses postpartum ovarian growth and follicular development.
Around half of cows with metritis will have a fever and most will be depressed and “off feed.” Eventually, the immune system regains its strength and will clear these infections. (Few cows actually die of metritis or endometritis.)
However, the inflammatory response required to gain the upper hand once the infection is established requires neutrophils, macrophages and lymphocytes, and is sustained beyond the periparturient period. This can cause enough damage to the mucosal cells lining the surface of the uterus (referred to as endometritis) that the cow has trouble becoming pregnant.
Estimates suggest a case of metritis costs about $106 per lactation in drug, veterinary services and lost production costs.
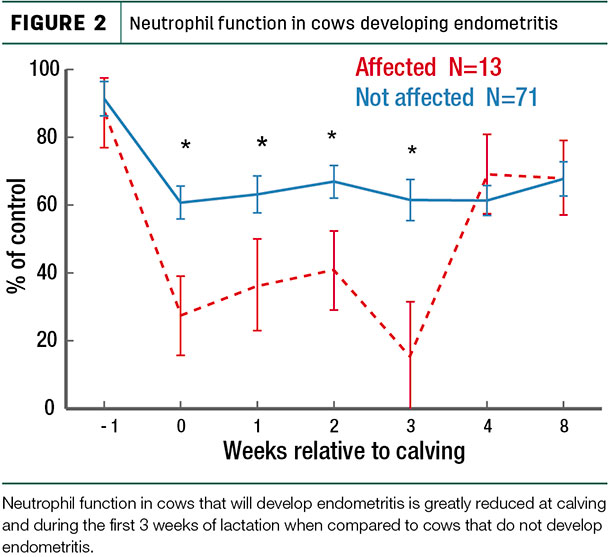
Working with Dr. Doug Hammon at Utah State, we were able to show that cows that would develop metritis between three and 10 days after calving had severely reduced neutrophil function the day they calved. In some cows, neutrophil function was depressed by 70 percent for the first four weeks of lactation as well. Those cows were diagnosed with endometritis at 28 days after calving due to persistent infections of the uterus (Figure 2).
Why are cows immune-suppressed around the time of calving?
The cow experiences tremendous changes in hormones around the time of calving. Estrogen rises dramatically the week before calving and has been shown to inhibit some lymphocyte functions. However, progesterone, which is very inhibitory to certain lymphocyte functions, declines just before calving.
Cortisol is secreted in low amounts as part of the initiation of the calving process. However, cortisol secretion can be extremely high in some cows – and at these levels, it will severely inhibit both neutrophil and lymphocyte function in the cow. Difficult or assisted calvings, severe hypocalcemia and overcrowding are common causes of cow stress that result in excessively high blood-cortisol levels.
The onset of milk production imposes tremendous challenges to the mechanisms responsible for energy, protein and mineral homeostasis in the cow. Negative energy, protein and/or mineral balance associated with the onset of lactation may be partially responsible for the immunosuppression observed in periparturient dairy cattle.
Using a mastectomized cow model, we were able to separate the effects of the hormonal changes around the time of calving from the effects metabolic stresses associated with the onset of lactation had on the immune system.
Those studies demonstrated that hormonal changes prior to calving caused neutrophil, but not lymphocyte, function loss during the two weeks before calving. After calving, the metabolic challenges associated with the onset of lactation reduced both neutrophil and lymphocyte function during the first two to three weeks of lactation. ![]()
Part 2 of this article series will cover hypocalcemia and ketosis, as well as steps to take to prevent immune suppression.
References omitted but are available upon request. Click here to email an editor.
Jesse Goff is a professor, Anderson Chair in Veterinary Medicine, College of Veterinary Medicine, Iowa State University, Ames, Iowa. Email Jesse Goff.






