We all know infectious diseases exist on dairies. They can present as an outbreak, be endemic in the herd or potentially both, and some cattle diseases may even pose a health risk to farm employees.
When faced with a new or recurring infectious disease, producers should monitor and record patterns in herd health, clinical signs in individual animals (including body temperature, appetite and attitude), treatments given (including doses and frequency) and response to treatment. Develop checklists or standard operating procedures (SOPs) for farm employees caring for sick animals. Provide this objective history to the herd veterinarian and analyze the information together to formulate an unbiased differential diagnosis list, or list of possible causes for the symptoms, then decide which animals to test.
It is ultimately the veterinarian’s responsibility to collect, prepare and submit appropriate samples to a veterinary diagnostic laboratory. Before submitting samples, consider what management changes can be implemented based on test results: “Can animals be culled? Can cleaning protocols be modified? Can new equipment be purchased?” Performing diagnostic testing without utilizing test results is a poor use of time and money.
Paperwork accompanying samples to the lab should describe a complete history of the farm, including age, breed, sex, herd management (housing, feeding, vaccine protocol, etc.) and all antibiotics administered. This will aid in accurate result interpretation.
Many infectious diseases have more than one type of test available for diagnosis. An antigen test detects the pathogen itself (bacteria, virus, fungus or parasite). The sample from the affected animal can be many different things, including feces, blood, a swab of a body part or tissues from a necropsy. An example of an antigen detection test is a fecal egg count for parasites on a manure sample or a milk culture from a mastitic cow. An antibody test, or titer, reflects the animal’s immune response to the pathogen or vaccine and is performed on a blood sample. Brucellosis testing detects antibodies to the bacteria Brucella abortus.
The type of test to perform (antigen versus antibody) can depend on the stage in the disease process. An acutely sick animal may be shedding the infectious agent but has not yet developed antibodies. A chronically ill or infected cow may have antibodies but no longer be shedding the pathogen. Calves under 4 months old have maternal antibodies from colostrum that can be detected on a blood sample. If an animal receives a modified-live vaccine and dies within a few weeks, tissue samples may test positive for the virus, but it is possible that the test may be detecting the vaccine instead.
Antibiotic treatment can kill bacteria and result in a negative bacterial culture. The variation in type of testing available and the timeframe of the disease process can impact the interpretation of lab results. This is another reason a complete history aids in getting the most accurate results possible.
Performing physical exams or necropsies on three or more animals and collecting samples is indicated when diagnosing an outbreak in a dairy herd. This is not a “magic” number, but more than two animals with the same disease process points to a pattern. If there are dead cattle, the herd veterinarian will perform a gross necropsy as soon as possible to maintain the integrity of the tissues before they begin to deteriorate.
A 3-centimeter-thick piece of each tissue should be placed in a separate sterile container to avoid cross-contamination. When collecting sections of the intestinal tract, especially for an animal that died of diarrhea, tying off a loop of intestine at each end will preserve the bacteria and allow for anaerobic culture in the laboratory. This is important if clostridium is a possible cause of diarrhea. (See top image.)
Another 0.5- to 1-centimeter-thick piece of each tissue should be placed in 10% buffered formalin (dilute formaldehyde) for histopathology, which is performed by a veterinary pathologist. The pathologist will examine fixed tissues under a microscope and write a report describing the disease process at the cellular level.
This information builds upon the gross necropsy performed on the farm as well as the interpretation of detecting pathogens through bacterial culture, PCR (polymerase chain reaction, which is a technique for detecting nucleic acids, or the “DNA” of a pathogen) or virus isolation (growing a virus in a liquid cell culture). (See images 2 to 4.)
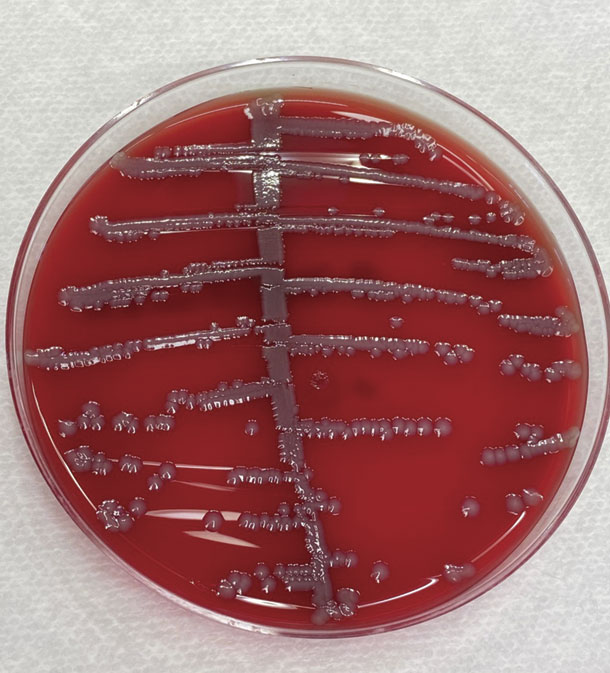
E. coli bacteria growing on a blood agar culture plate in a bacteriology lab. Photo courtesy of Rebecca Franklin-Guild.
For example, culturing E. coli bacteria from the intestine may not be significant because E. coli is part of the normal gut flora in all animals. If the pathologist finds evidence of bacteria-induced damage to the cells lining the intestinal wall, and E. coli is simultaneously cultured from the intestinal tract, this could indicate that E. coli is the cause of diarrhea. E. coli PCR genotyping can be performed on the E. coli bacterial colony grown in the laboratory.
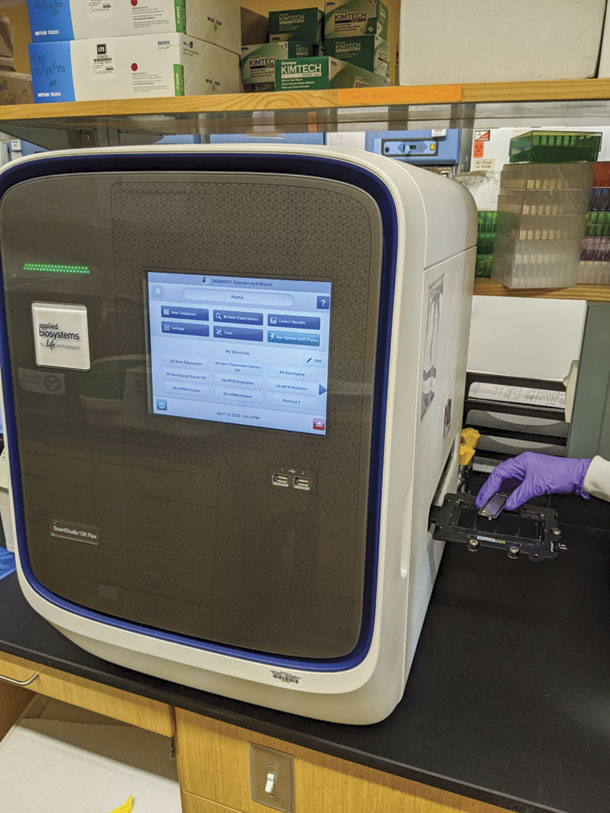
A laboratory technician loads a plate with very small aliquots of animal samples into the QuantStudio PCR machine. The machine will generate results within a few hours. Photo courtesy of John Beeby.
This PCR detects toxin-producing genes in the E. coli DNA, such as K99, F41 and shigatoxin, which are the toxins the E. coli bacteria release and wreak havoc on the gut. By combining the histology, culture and PCR genotyping results, we can demonstrate that the E. coli is significant.
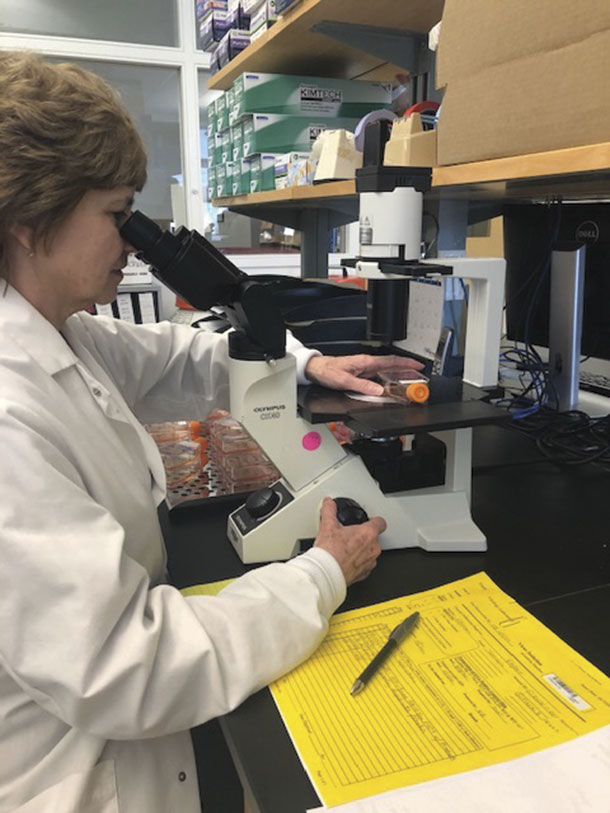
A laboratory technician examines a virus isolation flask with liquid cell culture media through a microscope. Photo courtesy of Jen Powers.
Veterinarians may also collect swabs of different organs and place them in transport media. Images 5 to 7 show proper technique for swabbing the intestinal lumen, which is the same procedure performed on a tied-off loop of intestine received in the laboratory.

A surgical scissor or necropsy knife is used to open a loop of intestine. Photo courtesy of Dr. Teresa Southard.

Once the intestinal lumen is open, ingesta is scraped from the mucosal surface, or inner lining of the intestine. Photo courtesy of Dr. Teresa Southard.

An 8- to 12-inch area of the intestinal mucosa is swabbed to collect a representative sample; then the swab is placed in appropriate transport media or plated directly in the laboratory. Photo courtesy of Dr. Teresa Southard.
Transport media (Image 8) allow preservation of fragile bacteria and viruses so they remain viable in transit to the veterinary diagnostic laboratory.

Different transport media available to veterinarians. From left to right: A plastic cup for individual fresh tissues, Anaerobic Transport Medium jar (for anaerobic and aerobic bacteria and fungus), BD BBL Port-A-Cul (also for anaerobic and aerobic bacteria and fungus), Para-Pak C&S for fecal specimens, Thermo Scientific VersaTREK EZ Draw aerobic blood culture vial (for sterile collection of blood in febrile animals), Viral Transport Medium (for virus isolation and PCR tests), Amies Transport Medium without charcoal (for aerobic bacteria only), Copan Diagnostics ESwab (appropriate for anaerobic and aerobic bacteria and PCR). Photo courtesy of Elisha Frye.
Fresh samples need to be refrigerated and sent for overnight delivery or frozen until they can be shipped overnight. Formalin fixed tissues and certain transport media, such as anaerobic transport media and blood culture vials, should remain at room temperature when being shipped. Once samples arrive, they are transferred to different sections of a full-service lab for various testing, depending on the information provided and tests requested on the submission form.
Veterinarians and staff at diagnostic laboratories are available to consult with field veterinarians on proper sample collection, test type and result interpretation. This maximizes the diagnostic capabilities for the dairy herd when faced with a herd health issue.