My inquisitive 11-year-old recently asked me if a newborn child belonging to a family we know was in the hospital because the baby didn’t get enough colostrum. Wow. I could tell by the look on his face it was going to be a long conversation when I told him human babies don’t need colostrum like calves do.
It occurred to me, the answer to his question also helped explain why retained placentas occur in cattle.
Cattle placentas have a total of six layers – three are fetal and three are maternal. As also with the horse and pig, this type of placenta is called an epitheliochorial placenta. The upside to this design is: The six layers form a very good barrier between the fetal and maternal blood.
Many blood inhabitants, like viruses and bacteria, are not able to gain passage from the mother to the fetus for this reason. Unfortunately, another blood inhabitant that cannot gain passage is immunoglobulins. For this reason, cattle need colostrum in order to gain immunoglobulins from the dam while human babies already have immunoglobulins from their mother at birth.
While cattle, horse and pig placentas all have six layers, there is a distinct difference between cattle placentas from the horse and pig placentas. This difference is whether the maternal components are sloughed during birth. An adeciduate placenta is one where the maternal component is not shed, as in the case of the horse and pig.
Cattle, however, have a partially deciduate placenta where part of the maternal component is shed. This design challenge lends cattle to be more prone to retained placentas.
Before leaving this anatomy lesson, there is one more piece of information to pass along. The cattle placenta has discrete placental junctions where apposition of the fetal and maternal layers are fused. We often call these the “buttons” on the uterus, which can easily be palpated in cattle in the third trimester.
These attachments are properly named placentomes. The fetal component is a cotyledon, which interdigitates with the maternal component called the caruncle. In order for the disconnection to occur, the maternal endothelium layer must be shed. If the events surrounding the pregnancy and delivery aren’t suitable, the maternal endothelium does not release; therefore the placentomes are still intact and a retained placenta occurs.
This last lesson is important to understand because the temptation in managing a retained placenta case is to simply manually remove it. When applying pressure and pulling apart the placentome, the blood vessels in these layers are torn. The process of tearing these attachments may lead to hemorrhaging.
Significant blood loss may occur in this process as well as scarring. Areas of scar tissue may not support the formation of placentomes for the next pregnancy. Without proper attachment and nutrient exchange, a fetus may not survive or properly develop.
So if not manual extraction, how then should a retained placenta be managed? Table 1 outlines some common options and a brief discussion of each follows.
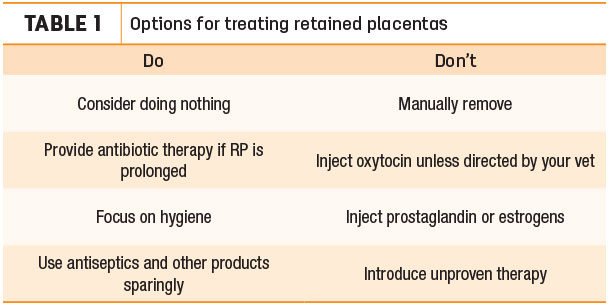
The choice to do nothing at the time of diagnosis of fetal membranes is common. The membranes at the site of attachment will eventually separate so the placenta can be expelled. This process may take days or weeks. Doing nothing does not imply the cow should not be monitored.
Instead, it should be closely monitored for systemic signs of disease. If these cattle are going to develop more complicated problems including infection, they will likely do so within a few days after a prompt diagnosis.
One indication of systemic infection is a rectal temperature exceeding 103ºF. Different health monitoring programs may differ on the exact temperature to implement treatment.
A point not mentioned in detail earlier is the ease of introducing contaminants into the uterus, which will cause a uterine infection. Cattle are six times more likely to have a uterine infection when the fetal membranes are retained as compared to cows without retained membranes.
Antibiotic therapy is often needed to treat retained placentas, especially if detachment is delayed. By definition, any fetal membranes attached longer than 24 hours post-parturition is considered a retained placenta. As mentioned before, the majority of cows with a retained placenta will develop a uterine infection, so systemic antibiotic therapy seems warranted.
However, it is important to note the treatment of such does nothing to aid in the detachment of the membranes, only to combat the infection present in the tissues.
Similar to sticking a needle in a sterile bottle of vaccine and setting it on a shelf, the retained placenta is a means for bacteria and contaminants to enter into the uterus. The membranes prevent the physical closure of the cervix, which provides a physical barrier to infectious agents gaining access to the uterus.
Oxytocin is the hormone of choice to initiate milk letdown as well as uterine contractions. Small amounts of oxytocin can be effective in causing immediate uterus contractions; however, too much oxytocin will result in spastic contractions.
Remembering that retained placentas are caused by the placentomes failing to loosen, the usefulness of increasing uterine contractions is debatable. Additionally, most cows with a retained placenta have normal to increased motility despite its use.
“The solution to pollution is dilution.” This was a favorite quote by many of my veterinary professors. The point to this is: Pollution, or infection, can be lessened by hygiene. Taking the time to trim fetal membranes so they do not drag in the manure, keeping manure cleaned off the vulva area and housing affected cows in dry and clean bedding are some ideas to diluting the pollution that can worsen the condition.
One note of caution is: Trimming the membranes too short may cause them to be pulled back into the uterus. There may be some value in keeping them farther outside the cow so they are weighted down and do not slip back inside the cow and introduce more contamination.
The usage of additional hormones like prostaglandin has been largely unsuccessful and controversial. Postpartum cows naturally have elevated levels of prostaglandin, which decline rapidly during the first eight days after calving and return to a basal level by 14 days after parturition.
There is no current evidence prostaglandin aids in the expulsion of retained fetal membranes. The use of estrogen is not supported because membrane expulsion and uterine involution occur when estrogen levels are low. Therefore, raising the estrogen levels would logically seem contraindicated.
The idea of using antiseptics is similar to the use of antibiotics in treating a retained placenta. The products aren’t to fix the problem but to address the ensuing infection. In most cases, effectiveness remains to be demonstrated. Additionally, many of these agents can be irritating or damaging to the uterine tissue. These treatments can inhibit the cow’s natural mechanisms in combating the condition.
Common products include hydrogen peroxide, chlorhexidine and iodine. Antibiotic use, as directly applied to the uterus, can also be placed into this category for this reason.
Single intrauterine applications of antibiotics often fail to prevent clinical metritis or to improve fertility in treated cows compared with untreated cows. There are multiple reasons why antibiotics are largely ineffective when given intrauterine.
First, dosages are too low to attain adequate tissue concentrations of antibiotics in the uterus by using uterine infusions. Next, the extreme pH of the antibiotic solutions may contribute damage to the uterus. Probably most importantly, there are no antibiotics labeled for an intrauterine route; therefore, usage is extra-label and would require consent from a veterinarian.
As such, withdrawal times are not established, leaving this practice largely a gamble with the risk of having a drug residue in a tank of milk.
While every once in a while a great idea comes along, a general rule of thumb is: If it sounds too good to be true, it probably is. Therefore, the likelihood a magic treatment for retained placenta will arise is slim. Research in the areas of collagenase treatments to break down the placentome by proteolysis and allow detachment has been somewhat successful.
Additional substances that trigger the activation of cotyledon proteases may be key to treatment of this condition. Many proposed solutions are time-consuming and financially expensive thus far.
Given the anatomy of the cow uterus, retained placentas are common compared to other species. Risk factors like periparturient hypocalcemia, dystocia, abortion, sex of the calf, twinning, stillbirth and the induction of parturition may impair neutrophil function and contribute to retained membranes. Intervention must be evaluated based on farm hygiene, incidence and ability to diagnosis early.
Your herd veterinarian is a necessary resource to guide treatment decisions and choices. Also, having an 11-year-old keeps one on one’s toes. You never know what will occur to you during a cow discussion. ![]()

-
Angela Daniels
- Veterinarian
- Circle H Headquarters LLC
- Email Angela Daniels