The cost of clinical and subclinical hypocalcemia is high – as numerous research studies and producer experiences prove. Thus, as with any disease that has no single cause, it is essential to focus on the risk factors associated with the disease and then reduce those risks to reduce disease incidence and expense.
Keep in mind these risk factors can be nutritional, but might also be related to housing and management. Therefore, don’t limit your investigative perspective to a single cause or single solution.
That said, consider the following nutritional factors as you develop your strategy to prevent hypocalcaemia in transition cows.
First things first
Don’t be misled by blood calcium cutoff points. Every cow will have a reduction in blood calcium around calving. This fact is often overlooked, but deserves attention. This means you must ask three pertinent questions during an assessment:
- When does the drop in blood calcium occur?
- How low does the blood calcium drop?
- How quickly do blood calcium levels return to normal postpartum?
Data for some of these questions related to the “average” cow exist, but making a clinical decision for an individual cow based on data averages can yield deceptive results – so don’t do it.
What has been learned is that some cows can drop blood calcium fairly low with no negative health implications, while others drop mildly and succumb to hypocalcemia. In fact, recent research points to the fact that cows (and mammals in general) may actually need a decline in blood calcium at calving to “kick start” metabolic processes to ensure a productive lactation.
What remains unknown is the magnitude, timing and duration of the decline in blood calcium necessary for a cow to become hypocalcemic. Therefore, declaring a blood calcium cutoff point to pronounce an individual cow hypocalcemic is generally an exercise in futility. The cutoff point will change with time after calving and also with adjustments in ration formulation, changes in acid-base status, differing levels of initial milk production and overall dairy management. Due to these factors, a blanket cutoff point can be deceptive.
Use up-to-date nutrition solutions
Nutritional solutions to minimize the risk for hypocalcemia are based on both current research and field trials. While historical data can be helpful at times, be sure to base any potential nutritional intervention on current findings.
Using older, outdated research can lead to further confusion and incorrect recommendations. While the cow’s metabolism has not changed over time, the dynamics of calcium metabolism have changed dramatically due to multiple factors, including:
- Dietary cation-anion difference (DCAD) was not considered prior to the 1980s.
- Cows now produce 80 pounds or more of milk per day in the first few days postpartum.
- Until fairly recently, the industry did not consider magnesium as a factor to minimize hypocalcemia.
Mining minerals for answers
Avoid confusing the issue by learning more about the finer points of feeding transition cows.
For instance, some are concerned that if cows are fed between 90 and 180 grams of calcium, cows will get hypocalcaemia. However, that’s not necessarily true. The research simply shows that the risk for hypocalcemia increases in this range by threefold. This has been shown in two independent studies, one in 1991 and one in 2006.
In addition, increased dietary magnesium (Mg) in today’s rations gives some nutritionists pause. But, there is research showing that Mg itself is a key nutrient that can predispose cows to hypocalcemia if dietary levels are too low. In the 2001 edition of the National Research Council (NRC) tables, the suggested requirement was increased to 0.35 to 0.40 percent Mg. Recent work would suggest that these values may need to be increased even further.
Lastly, there is a school of thought that suggests that it’s best to make prepartum diets as negative DCAD as possible to encourage increased blood calcium levels. However, feeding negative DCAD is needed to just acidify the cow’s blood. Once this is accomplished, there is no reason to acidify the blood further. Research has shown that the range of -8 to -12 meq per 100 g dry matter is usually sufficient to accomplish the task. Further, there is still debate on whether or not over acidifying (providing a more negative DCAD) will lead to metabolic issues after calving.
You’ll know when you’ve attained the desired level by monitoring the cow’s urine pH. Urine pH is the easiest measure as it directly reflects blood pH. There are protocols stating when to take samples and which cows should be sampled. (One such protocol is available on the Arm & Hammer Animal Nutrition website.)
Essentially, if more than 80 percent of Holsteins tested are averaging a urine pH of 6.5 or less (6.2 for Jerseys), the job is done. The protocol also has suggestions if you find excessive variation in this measure. Technically, any pH less than 7.0 is acid.
The reason that the suggested target values for urine pH are lower than 6.9 is to account for variation between cows and for variation in forage DCAD.
Ration considerations
Based on what researchers have learned over the past 40 years, here are the current recommendations for Holsteins:
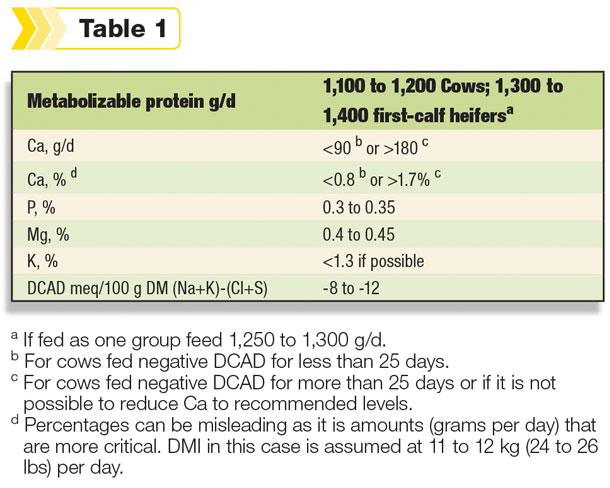
There is less data to make firm recommendations for Jerseys, but it is likely that dietary calcium will be at less than 60 g per day or greater than 150 g per day and metabolizable protein at 1,000 to 1,150 g per day.
Objective: Reduced risk
All of these recommendations and data are a collection of the latest research and field-tested experience intended to reduce the risk of hypocalcemia.
With any disease in any population of animals (humans included), disease can still occur even when following the best practices and recommendations, but the goal is to have it occur at a reduced frequency. Your objective should be to minimize the negative effects of hypocalcemia and increase the percentage of consistently good post-fresh outcomes.
As new research findings are published to help better understand metabolic issues and challenges, updated feeding recommendations will be put into place to help further reduce the risk of hypocalcemia and enhance transition health and performance. PD
References omitted but are available upon request. Click here to email an editor.
Elliot Block, Ph.D., is a research fellow for Arm & Hammer Animal Nutrition, and Neil Michael, DVM, is the global technical services manager for Arm & Hammer Animal Nutrition.
PHOTO: Risk factors for hypocalcemia include diet and nutrition, but might also be related to housing and management. Although disease can still occur, the goal is to reduce risk factors. Photo by Lynn Jaynes.







